Comprehensive Clinical Services for Cornea and External Eye Diseases
Cornea And External Eye Diseases
Beyond the Surface: Navigating Cornea Care with Precision

Cornea And External Eye Diseases
Beyond the Surface: Navigating Cornea Care with Precision
What are some diseases and disorders affecting the cornea and external eye?
As diabetes is a systemic disease, optimal control of blood sugar as well as blood pressure and cholesterol levels are still very important in the treatment of diabetic retinopathy. However, progression of retinopathy may occur despite all medical efforts. If diabetic retinopathy is detected early, treatment with laser photocoagulation may stop continued damage. Even in the advanced stages of the disease, laser treatment can reduce the chance that a patient will have severe visual loss.
Laser treatment is used to seal or obliterate the abnormal leaking blood vessels. This procedure focuses a powerful beam of laser light onto the damaged retina. Small bursts of the laser energy seal leaking vessels and form tiny scars inside the eye. The scars reduce new vessel growth and cause existing ones to shrink and close. Laser treatments are usually carried out in an outpatient setting.

Eye redness and watering from conjunctivitis
Allergies affecting the eye are fairly common. The most common allergies are those related to pollen, particularly when the weather is warm and dry. Symptoms can include redness, itching, tearing, burning, stinging, and watery discharge, although they are not usually severe enough to require medical attention.
An increasing number of eye allergy cases are related to medications and contact lens wear. Also, animal hair and certain cosmetics, such as mascara, face creams, and eyebrow pencil, can cause allergies that affect the eye. Touching or rubbing eyes after handling nail polish, soaps, or chemicals may cause an allergic reaction. Some people have sensitivity to lip gloss and eye makeup. Allergy symptoms are temporary and can be eliminated by not having contact with the offending cosmetic or detergent.
Corneal Infections. Sometimes the cornea is damaged after a foreign object has penetrated the tissue, such as from a poke in the eye. At other times, bacteria or fungi from a contaminated contact lens can pass into the cornea. Situations like these can cause painful inflammation and corneal infections called keratitis. These infections can reduce visual clarity, produce corneal discharges, and perhaps erode the cornea. Corneal infections can also lead to corneal scarring, which can impair vision and may require a corneal transplant.

Infection of the cornea with diffuse eye redness and inflammation
As a general rule, the deeper the corneal infection, the more severe the symptoms and complications. It should be noted that corneal infections, although relatively infrequent, are the most serious complication of contact lens wear.
Infection of the cornea with diffuse eye redness and inflammation
Dry Eye. The continuous production and drainage of tears is important to the eye’s health. Tears keep the eye moist, help wounds heal, and protect against eye infection. In people with dry eye, the eye produces fewer or less quality tears and is unable to keep its surface lubricated and comfortable.As we age, the eyes usually produce fewer tears. Also, in some cases, the lipid and mucus layers produced by the eye are of such poor quality that tears cannot remain in the eye long enough to keep the eye sufficiently lubricated. The main symptom of dry eye is usually a scratchy or sandy feeling as if something is in the eye. Other symptoms may include stinging or burning of the eye; episodes of excess tearing that follow periods of very dry sensation; a stringy discharge from the eye; pain and redness of the eye. Sometimes people with dry eye experience heaviness of the eyelids or blurred, changing, or decreased vision, although loss of vision is uncommon.
Dry eye is more common in women, especially after menopause. Surprisingly, some people with dry eye may have tears that run down their cheeks. This is because the eye may be producing less of the lipid and mucus layers of the tear film, which help keep tears in the eye. When this happens, tears do not stay in the eye long enough to thoroughly moisten it.
Herpes Zoster (Shingles). This infection is produced by the varicella-zoster virus, the same virus that causes chickenpox. Varicella-zoster virus may travel to the head and neck, perhaps involving an eye, part of the nose, cheek, and forehead. In about 40 percent of those with shingles in these areas, the virus infects the cornea.
Be aware that corneal problems may arise months after the shingles are gone. For this reason, it is important that people who have had facial shingles schedule follow-up eye examinations.
Herpes of the eye, or ocular herpes, is a recurrent viral infection that is caused by the herpes simplex virus. Ocular herpes can produce a painful sore on the eyelid or surface of the eye and cause inflammation of the cornea. Prompt treatment with anti-viral drugs helps to stop the herpes virus from multiplying and destroying epithelial cells. However, the infection may spread deeper into the cornea and develop into a more severe infection called stromal keratitis, which causes the body’s immune system to attack and destroy stromal cells. Stromal keratitis is more difficult to treat than less severe ocular herpes infections. Recurrent episodes of stromal keratitis can cause scarring of the cornea, which can lead to loss of vision and possibly blindness.
Keratoconus. This disorder–a progressive thinning of the cornea–is the most common corneal dystrophy in the U.S., affecting one in every 2000 Americans. In our population, it tends to occur more commonly in the Indian race. It is more prevalent in teenagers and adults in their 20s. Keratoconus arises when the middle of the cornea thins and gradually bulges outward, forming a rounded cone shape. This abnormal curvature changes the cornea’s refractive power, producing moderate to severe distortion (astigmatism) and blurriness (nearsightedness) of vision. Keratoconus may also cause swelling and a sight-impairing scarring of the tissue.
Studies indicate that keratoconus stems from one of several possible causes:
An inherited corneal abnormality. About seven percent of those with the condition have a family history of keratoconus.
An eye injury, i.e., excessive eye rubbing or wearing hard contact lenses for many years.
Certain eye diseases, such as retinitis pigmentosa, retinopathy of prematurity, and vernal keratoconjunctivitis.
Pterygium. A pterygium is a pinkish, triangular-shaped tissue growth on the cornea. Some pterygia grow slowly throughout a person’s life, while others stop growing after a certain point. A pterygium rarely grows so large that it begins to cover the pupil. Pterygia are more common in sunny climates and in the 20-40 age group. In areas where sunlight is strong, wearing protective eyeglasses, sunglasses, and/or hats with brims are suggested. While some studies report a higher prevalence of pterygia in men than in women, this may reflect different rates of exposure to UV light.
Pterygium in a patient’s left eye
Treatment of pterygia involve a relatively minor surgical procedure to remove the growth and placing a conjunctival graft (taken from the same eye) in its place to reduce the rate of recurrence. Nowadays, it is very common to use a special type of glue to secure the graft (rather than stitches) and this allows much more comfort and faster recovery for the patient.
What conditions may cause the need for a Corneal Transplant?
- corneal failure after other eye surgery
- keratoconus, a steep curving of the cornea
- hereditary corneal failure, such as Fuchs dystrophy
- scarring after infections, especially after herpes
- rejection after a first corneal transplant
- scarring after injury
In corneal transplant surgery, the surgeon removes the central portion of the cloudy cornea and replaces it with a clear cornea, usually donated through an eye bank. A trephine, an instrument like a cookie cutter, is used to remove the cloudy cornea. The surgeon places the new cornea in the opening and sews it with a very fine thread.
The thread stays in for months or even years until the eye heals properly (removing the thread is quite simple and can easily be done in an ophthalmologist’s office). Following surgery, eye drops to help promote healing and to prevent rejection of donor tissue will be needed for many months.
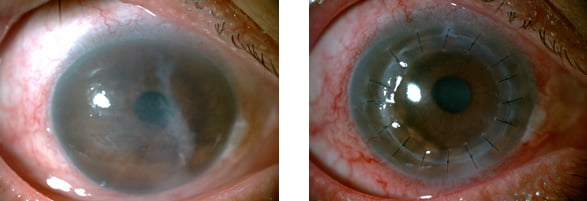
1 month post pterygium surgery – no stitches used
Modern technology for Corneal Transplant
Femtosecond Laser
By using the laser, a highly precise incision is created, resulting in a perfect match of the donor and the patient. In addition to precision that exceeds anything that can be duplicated by even a highly skilled surgeon, the laser can create complex shapes that are impossible to achieve with conventional surgery.
Femtosecond laser cutting of corneal tissue appears to be the way forward with a lot of experimental, preclinical and clinical research having demonstrated its effectiveness and safety. At LEC, our Wavelight Refractive Suite is capable of performing precise laser incisions for corneal transplants.
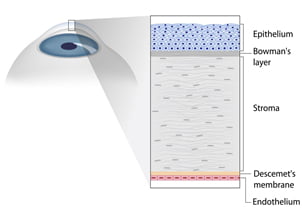
Structure of the cornea – 5 layers as shown
Frequently Asked Questions (FAQs)
Answers to Your Frequently Asked Questions: Clearing Up Common Queries
The cornea is the eye’s outermost layer. It is the clear, dome-shaped surface that covers the front of the eye.
Because the cornea is as smooth and clear as glass but is strong and durable, it helps the eye in two ways:
It helps to shield the rest of the eye from germs, dust, and other harmful matter. The cornea shares this protective task with the eyelids, the eye socket, tears, and the sclera, or white part of the eye.
The cornea acts as the eye’s outermost lens. It functions like a window that controls and focuses the entry of light into the eye. The cornea contributes between 65-75 percent of the eye’s total focusing power.
Conjunctivitis (Red Eye). This term describes a group of diseases that cause swelling, itching, burning, and redness of the conjunctiva, the protective membrane that lines the eyelids and covers exposed areas of the sclera, or white of the eye. Conjunctivitis can spread from one person to another. Conjunctivitis can be caused by a bacterial or viral infection, allergy, environmental irritants, a contact lens product, eyedrops, or eye ointments.
At its onset, conjunctivitis is usually painless and does not adversely affect vision. The infection will clear in most cases without requiring medical care. But for some forms of conjunctivitis, treatment will be needed. If treatment is delayed, the infection may worsen and cause corneal inflammation and a loss of vision.
A corneal transplant involves replacing a diseased or scarred cornea with a new one. When the cornea becomes cloudy, light cannot penetrate the eye to reach the light-sensitive retina. Poor vision or blindness may result.
See Our More Clinical Services

Cataract

Glaucoma

Diabetic Retinopathy

Retinal Diseases & Vitrectomy

Cataract

Glaucoma

Diabetic Retinopathy

Retinal Diseases & Vitrectomy
Get In Touch
If you are interested in talking to us about our clinical services, please send us a message.
